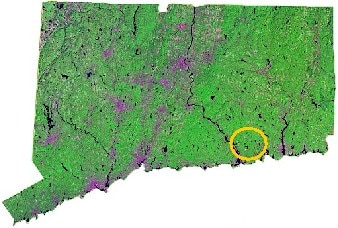
The Connecticut Department of Public Health, Epidemiology and Emerging Infections Program has maintained one of the most comprehensive Lyme disease surveillance systems in the country for approximately 30 years. Surveillance has included passive and active methods that incorporated physician-reporting and laboratory-reporting components. Surveillance methods were conducted statewide with the exception of active physician-based surveillance, which was limited to selected areas.
The history of Lyme disease in Connecticut began in 1975 when a cluster of children and adults residing in the Lyme, Connecticut area experienced uncommon arthritic symptoms. By 1977, the first 51 cases of Lyme arthritis were described, and the Ixodes scapularis (black-legged) tick was linked to the transmission of the disease. During 1982, Borrelia burgdorferi, the bacterium that causes Lyme disease, was discovered and the first brochure addressing Lyme disease was developed by the Arthritis Foundation. Serology testing became widely available in Connecticut during 1984. In 1987, Lyme disease became a reportable disease. All physicians were required to report any and all cases of the disease. By 1988, the news of Lyme disease spread and national media attention began. The first federal funding for Lyme disease surveillance, education, and research became available in 1991. The first Lyme disease vaccine became available in 1997. To help determine the efficacy of the vaccine, Lyme disease was made laboratory reportable in 1998. However, the manufacturer withdrew the vaccine from the market in 2001. In 2002, the vaccine efficacy study ended, and Lyme disease was removed from the list of laboratory reportable findings; however, it remained a physician reportable disease.
To help meet the program's mission, The Epidemiology and Emerging Infections Program will continue to maintain surveillance for Lyme disease. Surveillance methods may change over time to meet future needs. A statewide electronic laboratory reporting system, which will include Lyme disease, is being developed.
What is Lyme disease?
Lyme disease is an illness caused by the bacterium, Borrelia burgdorferi.
How is Lyme disease spread?
The bacteria are spread by the bite of infected Ixodes scapularis (black-legged) ticks. In Connecticut, these ticks are also commonly known as deer ticks. When in its nymphal stage, the tick is about the size of a poppy seed or the period at the end of this sentence. Not all deer ticks are infected.
Who gets Lyme disease?
Anyone can get Lyme disease; however, it is more prevalent in children < 10 years old.
What are the symptoms of Lyme disease?
Early Lyme disease symptoms include an expanding red rash that may appear around the area of the tick bite. The rash can resemble a bull's eye with a clearing center and distinct ring around it. Other early symptoms may include flu-like symptoms: fatigue, headache, fever, and achy muscles and joints. Later symptoms may include arthritis, neurologic problems, and heart problems.
How soon do symptoms appear?
The early symptoms of Lyme disease usually occur within the first month after the tick bite. Later symptoms can occur several weeks to several months later.
How is Lyme disease diagnosed?
Lyme disease may be difficult to diagnose because the symptoms can mimic many other disorders. Blood tests can be helpful in the diagnosis of Lyme disease but should not be used exclusively. Physicians will consider symptoms, history of tick bite, and the possibility of coming in contact with ticks to help in the diagnosis. If Lyme disease is suspected as the cause of illness, it is important that medical attention be sought.
What is the treatment for Lyme disease?
Lyme disease is easily treated when detected in the early stages. Treatment with oral antibiotics, such as doxycycline or amoxicillin, taken for a few weeks are often effective. Intravenous antibiotic treatment may be necessary for patients with late symptoms of Lyme disease.
How can Lyme disease be prevented?
To prevent Lyme disease and other tick-borne infections, the best protection is to avoid contact with ticks. When working or playing outside in areas that ticks inhabit (tall grass and weeds, woods, and leaf litter) you should:
Wear light colored clothing (to spot the ticks easily), long sleeved shirts and long pants.
Create a "tick barrier" by tucking pants into socks and shirt into pants.
Consider using insect repellent, according to manufacturer's instructions, when planning to be outdoors.
Check clothing and skin very carefully after being outdoors in tick infested areas.
Remove any ticks as soon as possible after they are discovered.
Keep your lawn mowed, cut overgrown brush, and clear any leaf litter away from the home.
Use a wood chip barrier between any wooded area and the yard.
Inspect pets daily and remove any ticks found.
How should a tick be removed?
It is important that a tick is removed as soon as it is discovered using tweezers. Grasp the tick mouth parts as close to the skin as possible and pull the tick out with steady pressure. Do not yank the tick out. Do not crush the ticks body with the tweezers as it may contain infectious fluids.
Do not use petroleum jelly, hot matches, nail polish remover, or any other substance to remove a tick. By using these substances, you may actually increase your chance of infection.
Thoroughly wash the area of the bite with soap and water and put an antiseptic on it.
The sooner the tick is removed, the lesser the risk of tick-borne infection. Research has found that infected ticks need to feed for 24-36 hours before transmission occurs.
Write on the calendar the date you removed the tick and the part of the body it was removed from. Check this area daily for 30 days.
Contact your physician if you believe you are experiencing symptoms of Lyme disease for recommendations on testing and treatment.
This fact sheet is for informational purposes only. It should not be used for self-diagnosis or as a substitute for consultation with a health care provider. If you think that you may have this infection, or have questions about the disease described above, you should consult your health care provider.
Lyme disease is an illness caused by the bacterium, Borrelia burgdorferi.
How is Lyme disease spread?
The bacteria are spread by the bite of infected Ixodes scapularis (black-legged) ticks. In Connecticut, these ticks are also commonly known as deer ticks. When in its nymphal stage, the tick is about the size of a poppy seed or the period at the end of this sentence. Not all deer ticks are infected.
Who gets Lyme disease?
Anyone can get Lyme disease; however, it is more prevalent in children < 10 years old.
What are the symptoms of Lyme disease?
Early Lyme disease symptoms include an expanding red rash that may appear around the area of the tick bite. The rash can resemble a bull's eye with a clearing center and distinct ring around it. Other early symptoms may include flu-like symptoms: fatigue, headache, fever, and achy muscles and joints. Later symptoms may include arthritis, neurologic problems, and heart problems.
How soon do symptoms appear?
The early symptoms of Lyme disease usually occur within the first month after the tick bite. Later symptoms can occur several weeks to several months later.
How is Lyme disease diagnosed?
Lyme disease may be difficult to diagnose because the symptoms can mimic many other disorders. Blood tests can be helpful in the diagnosis of Lyme disease but should not be used exclusively. Physicians will consider symptoms, history of tick bite, and the possibility of coming in contact with ticks to help in the diagnosis. If Lyme disease is suspected as the cause of illness, it is important that medical attention be sought.
What is the treatment for Lyme disease?
Lyme disease is easily treated when detected in the early stages. Treatment with oral antibiotics, such as doxycycline or amoxicillin, taken for a few weeks are often effective. Intravenous antibiotic treatment may be necessary for patients with late symptoms of Lyme disease.
How can Lyme disease be prevented?
To prevent Lyme disease and other tick-borne infections, the best protection is to avoid contact with ticks. When working or playing outside in areas that ticks inhabit (tall grass and weeds, woods, and leaf litter) you should:
Wear light colored clothing (to spot the ticks easily), long sleeved shirts and long pants.
Create a "tick barrier" by tucking pants into socks and shirt into pants.
Consider using insect repellent, according to manufacturer's instructions, when planning to be outdoors.
Check clothing and skin very carefully after being outdoors in tick infested areas.
Remove any ticks as soon as possible after they are discovered.
Keep your lawn mowed, cut overgrown brush, and clear any leaf litter away from the home.
Use a wood chip barrier between any wooded area and the yard.
Inspect pets daily and remove any ticks found.
How should a tick be removed?
It is important that a tick is removed as soon as it is discovered using tweezers. Grasp the tick mouth parts as close to the skin as possible and pull the tick out with steady pressure. Do not yank the tick out. Do not crush the ticks body with the tweezers as it may contain infectious fluids.
Do not use petroleum jelly, hot matches, nail polish remover, or any other substance to remove a tick. By using these substances, you may actually increase your chance of infection.
Thoroughly wash the area of the bite with soap and water and put an antiseptic on it.
The sooner the tick is removed, the lesser the risk of tick-borne infection. Research has found that infected ticks need to feed for 24-36 hours before transmission occurs.
Write on the calendar the date you removed the tick and the part of the body it was removed from. Check this area daily for 30 days.
Contact your physician if you believe you are experiencing symptoms of Lyme disease for recommendations on testing and treatment.
This fact sheet is for informational purposes only. It should not be used for self-diagnosis or as a substitute for consultation with a health care provider. If you think that you may have this infection, or have questions about the disease described above, you should consult your health care provider.